Diabetic retinopathy
Diabetic retinopathy is the damage caused by diabetes to the retina. It is the most common cause of blindness in people under the age of 50 in Australia.
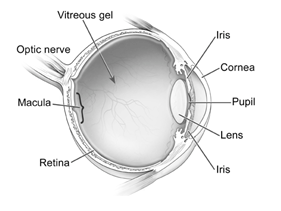
Diabetes damages the small blood vessels that supply the retina. The retina is a thin layer of light sensitive tissue that lines the back of the eye. Damage to the blood vessels causes visible changes such as bleeding or cholesterol deposition (diabetic retinopathy). The macular is a small area at the centre of the retina. The macular is responsible for central vision.
Diabetic retinopathy can develop in anyone who has either type 1 or type 2 diabetes. The longer you have diabetes and the less controlled your blood sugar is, the more likely you are to develop this complication. Poor control of blood pressure and cholesterol levels can also increase your risk of developing diabetic retinopathy.
Symptoms
Initially diabetic retinopathy may cause no symptoms or very mild symptoms. So diabetic retinopathy often goes unnoticed in the early stages. This is why
diabetics should have at least an annual dilated retina examination
Don’t wait for symptoms
As the condition progresses diabetic retinopathy usually causes visual loss that in many cases cannot be reversed
symptoms can include:
vision loss
spots or dark strings (floaters)
blurred vision
fluctuating vision
impaired colour vision
dark/empty areas in your vision
Stages of retinopathy
Non proliferative diabetic retinopathy (NPDR)
This is the earliest stage of diabetic retinopathy.
Blood vessel walls in the retina weaken and can cause small areas of balloon like swellings (microaneurysms).
The buldges often leak:
– tiny spots of blood leak into the retina (retinal hemorrhages)
– cholesterol and other fats from the blood (hard exudates)
To see a simulation of what vision with non proliferative diabetic retinopathy can look like when it affects vision click below.
Diabetic maculopathy
Leaking fluid can cause the macular to swell/thicken (diabetic macular edema = DME) causing a loss in central vision.
Diabetes can also cause the small blood vessels to close and restrict blood flow to the macular (macular ischemia) which also causes affected vision.
Proliferative Diabetic Retinopathy (PDR)
Non proliferative diabetic retinopathy can progress over time to the next stage of the disease called proliferative diabetic retinopathy (new blood vessels growing). Abnormal fragile blood vessels grow on the surface of the retina. These vessels can leak into the vitreous (vitreous haemorrhage). If the haemorrhage is small it can be seen as dark floaters. If it is a large bleed it can block vision only allowing light and dark discrimination. The abnormal vessels can become scar tissue that pulls on the retina resulting in the retina becoming detached from the wall of the eye (tractional retinal detachment). If the new blood vessels restrict the normal flow of fluid out of the eye, pressure can build up which can cause damage to the optic nerve (neovascular glaucoma).
To see a simulation of what vision with proliferative diabetic retinopathy can look like when it affects vision click below.